In This Issue:
- New Report Examines the State of Locum Tenens in 2023: Key Trends and Insights
- A Look into Aspirus Health and UnityPoint Health’s Efficient Locum Tenens Hiring
- Medicus: 10 Strategies for Seamlessly Integrating Permanent and Locum Tenens Staff
- Floyd Lee Locums Celebrates Expanded Charleston Headquarters
- AMA: Restoring Joy in Medicine Through Small Changes
- 15 Trailblazing Ideas to Improve Healthcare by 15 Leading Thinkers
- Webinar: Physician Recruitment Strategies in 2023- What You Need to Know
- Tomorrow’s Success Starts Today: The Importance of Multiple Talent Strategies
- Fixing the Workplace, Not the Worker: The Key to Addressing the Root Cause of Doctor Burnout Prevention
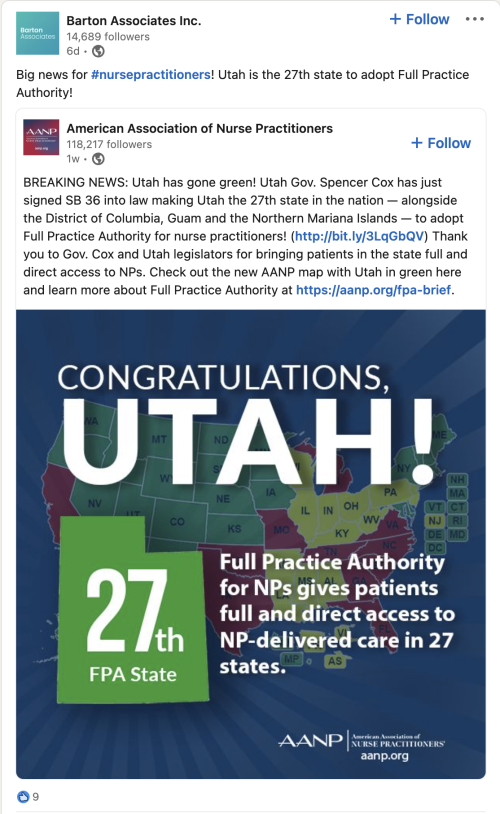
- Socially Speaking: Social posts of note from Medicus, Weatherby, Barton Associates, Jackson+Coker, & more.
- 9 Initiatives Tackling Physician Burnout
- Three Ways Digitalization Is Transforming Healthcare
CHG Report Examines the State of Locum Tenens in 2023: Key Trends and Insights
(From CHG Healthcare, 3/21/2023)
CHG Healthcare, the country’s largest provider of locum tenens staffing services, recently released its “2023 State of Locum Tenens” report, an overview of current short-term staffing trends. The report highlights a significant increase in physicians taking locum tenens assignments, particularly among early-career physicians seeking better work-life balance.
According to the report, approximately 7% of physicians, or 50,000, have worked at least one locum assignment in the past year, an 88% increase since 2015. Of those physicians with locum tenens experience, 43% work full-time compared to 30% in 2019.
Luke Woodyard, president of Weatherby Healthcare, which is owned by CHG, noted that “locums in the past were typically older, more tenured physicians looking for a way to ease into retirement. Today, we’re seeing more and more young physicians who want better work-life balance and flexibility in their lives. Being a physician used to be all about the work; now it’s about the work and the life outside of work.”About 59% of physicians with locum tenens experience reported taking their first assignment within a decade of finishing their medical training. Physicians practicing locum tenens earlier in their careers primarily do so for better work-life balance. Most of the locum tenens workforce consists of mid-to-late career physicians over age 45.
Rising Utilization of Locum Tenens by Healthcare Facilities
Healthcare facilities use locum tenens for myriad reasons, such as maintaining patient access to care and filling temporary vacant positions for clinicians on family leave or vacation. Since 2020, CHG’s report found that more facilities are utilizing locums to meet the rising patient demand during peak periods, such as flu season.
“Our system is big enough that we are able to offer our patients a wide variety of services, said Amy Powell, CPRP, Director of Medical Staff Recruitment at Reid Health, a not-for-profit health system with over 200 beds in its inpatient hospital in Richmond, Indiana. “However, we’re small enough that if one or two people leave, we can feel a significant strain on staffing. Locum tenens lets us cover those gaps and offer our patients the care they expect.”
According to the report, 64% of surveyed organizations used locum tenens, and 84% stated that their utilization of locum tenens would remain constant or increase in the future.
Locum Tenens Received Positively Across Healthcare Industry
The report also delved into physicians’, patients’, staffing personnel’s, and colleagues’ perceptions of locum tenens. Seventy-one percent of physicians reported having “very positive” or “somewhat positive” impressions of locum tenens. Favorable impressions remained constant over the past few years.
Hospital staffing personnel reported a high acceptance of locum tenens usage in their facilities, with some even embracing the model. Administrative staff (79%) and physician colleagues (76%) stated they accepted locums physicians; 16% and 13% of those groups, respectively, embrace the model.
Melinda Giese, SVP of CHG Healthcare, highlighted how “health systems can benefit in three ways: strategically approaching locum tenens staffing, utilizing telehealth and technology for patient care accessibility, and addressing physician burnout. Locum tenens should be viewed as a profit center, generating up to three times their cost. This approach offers flexibility to physicians and staff and serves as a valuable short-term solution to healthcare access and workforce shortages.”
The report underscores the need for flexible staffing solutions such as locum tenens to address the ongoing healthcare workforce shortage and meet rising patient demand. While locum tenens may not be a universal solution, it can offer value as a short-term or interim solution that provides flexibility to physicians and their overburdened permanent staff.
La Vida Locum
A Look into Aspirus Health and UnityPoint Health’s Efficient Locum Tenens Hiring
(From CHG Healthcare, 3/14/2023)
A recent CHG Healthcare blog post discussed how Aspirus Health and UnityPoint centralized their locum tenens hiring processes to improve efficiency, reduce redundancies, and save money.
Aspirus Health, which focuses on rural healthcare, moved one location or group to a centralized model at a time. Located in Iowa, Illinois, and Wisconsin, UnityPoint Health, centralized its locum tenens hiring utilizing a Lean process that prioritizes customer value by creating streamlined processes and minimizing waste.
Streamlining Locum Tenens Hiring Through Centralization
Centralization has numerous benefits, including streamlined hiring, reduced locums credentialing time, ensured continuity of care, and better monitoring of spending. It has also reduced the number of locum tenens agency partners, allowing for more robust relationships with the partners who best fit their needs. By reducing redundancy and inefficiencies, centralization has created a pool of locums for each specialty to go to each organization’s locations.
Building Stronger Bonds with Agency Partners
Through the centralization process, UnityPoint ended up reducing the number of its locum tenens agency partners to one primary agency and a tiny handful of specialty partners. Aspirus saw a reduction from roughly 20 partners to about 10.
For both organizations, reducing the number of agency partners has helped build stronger relationships with the partners who best fit their needs.
The agencies that continued to partner with Aspirus demonstrated a thorough understanding of which candidates would be compatible with them.
Going the Extra Mile
Centralization may require time and effort, but the benefits include reduced costs, increased efficiency, and the reallocation of resources for greater effectiveness. The process has also reduced the time and money spent on orientation for new locum providers.
Aspirus and UnityPoint have seen positive results from centralizing their locum tenens hiring processes, even though they used different approaches.
Medicus: 10 Strategies for Seamlessly Integrating Permanent and Locum Tenens Staff
(From Medicus Healthcare Solutions, 3/14/2023)
Medicus Healthcare Solutions highlighted in a recent blog post the increasing importance of locum tenens providers in healthcare staffing, particularly as the demand for physicians and advanced practitioners continues to rise.
However, more than just filling staffing gaps is required for healthcare employers to provide the best patient care. To do so, healthcare employers must integrate permanent and locum tenens staff into their teams, ensuring that both groups are a fit, clinically and culturally. This includes providing information, resources, and assistance before a locum tenens provider’s start date is crucial for a seamless experience and developing a cohesive healthcare team.
To facilitate a strong connection between permanent locum tenens staff, Medicus suggests these 10 strategies:
- Notify permanent staff of locum tenens arrival and the provider’s unique skillsets.
- Welcome locum tenens as team members and assign a “buddy”.
- Provide adequate training for faster contribution toward team goals.
- Introduce locum tenens to permanent staff and encourage communication.
- For unity, focus communication on high-quality care.
- Ensure consistent and equitable communication with all staff.
- Be intentional and inclusive with social engagement.
- Encourage attendance and participation at meetings and uplift input.
- Arrange team events with icebreakers, such as lunch.
- Celebrate diversity by appreciating unique backgrounds and perspectives.
Locum Leaders
Floyd Lee Locums Celebrates Expanded Headquarters
(From Floyd Lee Locums, 3/13/2023)
On March 14, Floyd Lee Locums celebrated the expansion of its Charleston, SC, headquarters office in conjunction with the company’s sixth anniversary.
The ribbon-cutting ceremony was officiated by North Charleston Mayor, R. Keith Summey. Floyd Lee COO Nicole Burleson, VP of Engagement Tim Rogers, and other community leaders delivered speeches while live music played and office tours were given.
“We are thrilled to have a new presence in Charleston that reflects our commitment to growth and continuing to deliver on our mission of connecting clinicians to purposeful work,” said CEO Natasha Lee. “Our new space enables us to better serve our healthcare providers and clients nationwide and better engage with our local community.”
The ribbon-cutting ceremony was captured below. Additional photos of the ceremony can be viewed on LinkedIn.

Hire Power
AMA: Restoring Joy in Medicine Through Small Changes
(From American Medical Association, 3/14/2023)
As an American Medical Association news story notes, medical groups are employing various strategies to address the physician burnout crisis. Permanente Medical Group in Oakland, California, used a survey to gather data on workload, wellness, clerical and administrative burdens, professional development, and psychological safety. Based on the data, department chiefs asked technology leaders to coach physicians using voice dictation and creating templates to reduce charting time.
Permanente received recognition from the AMA Joy in Medicine™ Health System Recognition Program for its campaign to improve physician well-being. Amanjot Sethi, MD, who directs wellness operations, explained a three-part framework they adopted to ease physician burdens and foster teamwork.
- The first key element of the framework was practice support, which optimized systems and tools, allowing physicians to spend more time on meaningful and purpose-driven work.
- The second element was culture, which looked at how the health system chose its leaders, developed skills to lead in a collaborative environment, and offered professional development opportunities for its people across their career arc.
- The third element was personal wellness, creating diverse, unique wellness programs to help doctors and physicians prioritize their health.
Dr. Sethi emphasized that an effective strategy depends on setting goals and putting the plan in motion, ensuring all operational leaders use the framework to speak the same language and identify strengths and opportunities in their domains. Undertaking a task of this scope can be challenging. Dr. Sethi and his team supported leaders by providing tools and skill-building to help them navigate conversations within their departments and spheres of influence.
Small interventions, such as the orthopedics department’s targeting of physical therapy orders as the most impactful administrative burden, can make a big difference. Department personnel worked together to develop new ordering templates so that their medical assistants could easily input the orders based on the type of patient being treated.
Dr. Sethi believes that physicians can restore joy in medicine by looking at work as physicians and thinking about their long-term health and sustainability.
Making the Rounds
15 Trailblazing Ideas to Improve Healthcare by 15 Leading Thinkers
(From Forbes, 3/20/2023)
The former CEO of Kaiser Permanente, George Halvorson, launched the Fixing Healthcare podcast in 2018, hoping to improve healthcare by achieving the same quality, technology, and affordability his medical group delivered to 5 million patients. Over the past five years, the podcast has featured dozens of leaders, thinkers, and doers in and around medicine who have shared innovative ideas and offered proven solutions to improve patient access, lower overall costs, and have great patient and clinical outcomes satisfaction.
Halvorson shared 15 top recommendations for improving healthcare over 150 episodes, including rewarding better care, integrating delivery systems, changing the view of primary care, supporting healthcare infrastructure, addressing factors affecting health, and giving patients a voice in their medical bills.
Below is the list of experts’ opinions on the following:
Fixing the business of medicine:
1. Malcolm Gladwell: Reward those who do things better.
2. Richard Pollack: Focus on ensuring that people get care in a very convenient way.
Eliminating burnout:
3. Zubin Damania: Change negative perceptions of primary care.
4. Devi Shetty: Work to help society.
5. Jonathan Fisher: bridging these divides between institutions and specialties to work together.
Making Medicine Equitable:
6. Jen Gunter: Teach women’s health in medicine.
7. Amanda Calhoun: Work on rebuilding trust with the Black community.
Addressing social determinants of health:
8. Don Berwick: Invest in early childhood development, workplaces, support to elders, community infrastructures, anti-racism, and criminal-justice reform.
9. David T. Feinberg: Focus on factors that impact health: genetic code, zip code, social environment, access to clean food, transportation, and loneliness.
Empowering patients:
10. Elisabeth Rosenthal: Encourage patients to write about surprise medical bills.
11. Gordon Chen: Build relationships and earn patient trust to drive better health outcomes.
Utilizing technology:
12. Vinod Khosla: Use technology and AI to capture expertise and increase efficiency.
13. Rod Rohrich: Use social media to educate and empower patients.
Rethinking medical education:
14. Marty Makary: Eliminate useless curriculum.
15. Eric Topol: Make AI a core curriculum in medical schools.
Who will take charge of healthcare change?
Providers could demand payment reform, switching to a ” capitation ” model that pays based on quality rather than quantity, and encourages collaboration and prevention. Or retailers like Amazon, CVS, and Walmart may disrupt healthcare by investing in in-home care and using AI solutions like ChatGPT. Change is inevitable, with the healthcare system struggling and the pandemic highlighting its flaws. Will it come from within or outside the system?
Webinar: What You Need to Know about Physician Recruitment Strategies in 2023
(From Becker’s Hospital Review, 3/23/2023)
The recent webinar, “Evolution of Today’s Physician Recruitment Strategies: What to Consider in 2023,” hosted by Becker’s Hospital Review, featured two experts who shared their thoughts on recruitment and retention strategies for healthcare staffing organizations. The presenters were Andrea Nelson, President of VISTA Staffing Solutions, and Tammy Hager, Executive Director of Recruitment and Privileging at Surgical Affiliates Management Group.
The Association of American Medical Colleges (AAMC) noted that 2022 was the most challenging year for physician shortages. There weren’t enough physicians coming out of training to fill vacant spots, meaning that healthcare organizations need individual company plans. It is essential to consider what is important to the physicians they serve and to connect the physicians and hospitals to succeed. While compensation is not the primary driver, doctors want quality interactions with patients and organizations.
Recruitment innovation involves focusing on medical schools in rural areas to recruit physicians who have ties to those areas and finding new ways to attract physicians in the areas they serve. Retention motivators include addressing provider needs at the individual level, compensation no longer being the motivator it once was, and leadership development. It is also essential to understand the culture of the organization with which the physician will work. Retirement and the opportunity to have a similar role in a different facility are the primary drivers of physician turnover.
The desirability of the location impacts the use of locums, with those in less desirable locations more likely to use locum tenens for their search. Future strategies include partnering with a strategic partner to address the needs of the patients and communities they serve and a transparency component.
To build a committed physician workforce, hospitals and health systems must be thoughtful about their recruitment and retention strategies, balancing the voice of the physician and the demands of the balance sheet through collaboration and partnership. Healthcare organizations must focus on recruiting and retaining physicians amid a challenging economic environment and worsening physician shortage. By keeping communication open and remaining flexible, organizations can provide communities with the highest quality patient care while supporting physicians and their needs.
The webinar highlighted the importance of innovation, understanding the organization’s culture, addressing provider needs individually, and building a committed physician workforce through collaboration and partnership. Healthcare organizations must focus on recruiting and retaining physicians amid a challenging economic environment and worsening physician shortage.
By keeping communication open and remaining flexible, organizations can provide communities with the highest quality patient care while supporting physicians and their needs.
Tomorrow’s Success Starts Today: The Importance of Multiple Talent Strategies
(From Becker’s Hospital Review, 3/14/2023)
The healthcare industry faces significant workforce challenges, such as a shortage of nurses, increased burnout, and a rise in retirement plans. The pandemic further complicated this issue, as hiring rates are not keeping up with a turnover, and travel nurses are tired and exiting the temporary staffing pool.
Talent management strategies must adapt yet be in tune with the challenges healthcare organizations face today. Permanent staff is the foundation of any healthcare organization’s ability to provide care and services. A strategy that could help improve retention and engagement, especially among nurses, is to adopt team-based staffing models, pinpoint staff willing to receive cross-specialization training or offer shorter shifts. At the same time, outsourcing the external recruitment process can aid internal talent acquisition teams by streamlining a system’s internal recruiters, making the process more efficient.
Contingent staff, like float pools, traveling providers, and per diem agency caregivers, are the next layer of providers after permanent staff. The influx of bid-driven marketplaces allows healthcare facilities to staff and manage their entire range of contingent talent promptly. These marketplace systems are agency agnostic, allowing them to access hundreds of suppliers that submit qualified and available candidates for clinical and non-clinical talent needs, matched to each organization’s specific criteria.
Technology tools such as telemedicine and artificial intelligence are crucial components of an effective workforce management model and an organization’s ability to provide care. Furthermore, predictive analytics is increasingly used to schedule the workforce across a healthcare system or facility, boosting scheduling accuracy. As a result of the pandemic, telemedicine and artificial intelligence is being more widely accepted and adopted by many across the healthcare landscape.
Fixing the Workplace, Not the Worker: The Key to Addressing the Root Cause of Doctor Burnout Prevention
(From Chief Healthcare Executive, 3/10/2023)
Healthcare leaders came together during an American Medical Association (AMA) webinar to address the rising problem of physician burnout. A common thread throughout the discussion was doctors need to be allowed to focus on patient care and not spend excessive time on documentation and working day and night.
Putting the Spotlight on Workplace Improvement
In 2021, 63% of physicians experienced burnout. Healthcare leaders emphasize the need to improve the workplace rather than fixing the individual worker. Many doctors are considering leaving medicine, with up to one in five planning to do so within two years.
According to a survey by Medscape, administrative hassles are the top contributor to burnout. Health systems should find ways to reduce bureaucratic headaches, including examining electronic health record systems to gain insights into doctors’ time on documentation.
Measurable ways to reduce burdens and burnout need to be tracked. Doctors’ frustrations with prior authorization have also been cited, and the administration is pushing for reforms in this area. By investing upstream in improving the workplace, health systems can reduce the $13 million annual cost of replacing doctors due to burnout and see a strong return on investment.
Streamline Access to Assistance: Making Help More Accessible
The panelists highlighted the importance of reducing bureaucratic headaches and promoting a culture of easily accessible help for healthcare workers. Health systems should reinforce this message and provide convenient access to mental health professionals via telehealth.
Healthcare executives must set an example by sharing their experiences with burnout, depression, or anxiety, to encourage other clinicians to seek help without feeling weak. Nigel Girgrah, chief wellness officer & medical director of liver transplantation at Ochsner Health, shared his struggles with anxiety and depression during the webinar and disclosed his story in an open letter to Ochsner staff in September 2020.
Healthcare systems should offer rooms for mental health professionals and encourage healthcare workers to seek help. Healthcare executives must lead by example and share their stories to help normalize seeking help.
Supporting Physicians in a Challenging Healthcare Environment
The webinar aimed to eliminate burnout. Panelists addressed isolation, which can increase stress and burnout. Good relationships are essential, as some physicians feel lonely after training. Social connections are necessary.
Galion emphasized the importance of rest and reducing workloads to give doctors more sleep. A Jama Network Open study found that 29% of doctors had at least one sleep disorder, increasing the likelihood of burnout. Galion notes that adequate sleep is crucial for better cognitive performance.
Second Opinion
9 Initiatives Tackling Physician Burnout
(From Becker’s Hospital Review, 3/15/2023)
Physician burnout is causing staff shortages and changing the industry. A Medscape survey found that 23% of physicians are depressed, and 9% have suicidal thoughts. Workplace stressors, such as increased documentation requirements and a lack of support staff, have led to an exodus of physicians from the profession.
Physicians and hospitals are implementing new solutions to keep physicians in the field and bring joy back to the profession. Here are nine initiatives emerging from the crisis:
Physician initiatives
- 3 ways a Kaiser Permanente physician aims to restore joy in medicine
- Viewpoint: Why physicians are turning to side hustles
- Viewpoint: Improve physician resiliency with a ‘badness’ plan
Hospital and health system initiatives
- Expanding medical residency programs may help curb physician shortage
- 33 states where physicians can earn multistate licenses
- Are zero-tolerance policies for patient bias on the right track?
- AMA shares 3 tips for preventing violence in hospitals
- AdventHealth grows medical school partnerships
- Want to lower physician burnout by 26%? Hire a scribe, study says
Three Ways Digitalization Is Transforming Healthcare
(From Forbes, 3/16/2023)
The Covid-19 pandemic transformed the medical industry and created significant strains on hospitals and health systems, including labor shortages and healthcare worker burnout. As the physician shortage persists, healthcare providers must find ways to do more with fewer resources.
However, the pandemic also accelerated healthcare innovation and the role of technology in the future of healthcare. Here are three ways digital integration can enhance the patient experience and make practitioners more efficient.
1. The Role of Artificial Intelligence in Enhancing Medical Systems
AI is becoming increasingly influential in improving clinical outcomes in healthcare, with 59% of U.S. healthcare executives believing in its effectiveness. It can analyze patient data, spot patterns, predict outcomes, and identify potential health risks. AI’s next frontier is using patient data for analytical insights and remotely interpreting patient data in real time to augment human intervention and improve healthcare provider response times.
2. How Remote Patient Monitoring Brings Healthcare into the Home
Remote patient monitoring offers numerous benefits for patients, healthcare providers, and hospitals. By utilizing both hardware, such as wearable devices, and software that incorporates data processing and visualization, doctors can receive real-time alerts, allowing for timely intervention.
This technology helps improve patient outcomes, reduce hospital stays, and lower costs. Patients with chronic conditions benefit the most, as they can receive extensive vital sign monitoring in their environments, freeing up beds for in-person care.
3. Easing Clinician Burdens with Clinical Workflow Solutions
Clinical workflow solutions reduce clinician burdens. Even with technological advancements, healthcare must still be weighed down by paperwork and manual processes. Providers spend hours daily transferring written patient information between shifts, which can lead to errors and reduced time for direct patient care. The labor shortage exacerbates the problem, with 34% of physicians seeing increased medical errors.
These solutions can provide a central hub for patient data storage and retrieval using desktop terminals, mobile devices, and on-site medical equipment. This workflow enhances care quality and reduces medical errors by allowing healthcare providers to input patient data and care directly into digital systems.
Emerging Technologies and Trends of Healthcare 2.0
Future healthcare will feature data-driven, patient-centric tools that seamlessly integrate into care delivery, streamlining workflows and empowering providers to give individualized care. To achieve this, hospitals must involve critical stakeholders, including doctors and nurses, in the discussion to determine the best solutions for their specific needs.
It is also vital to assess current IT infrastructure to ensure it can handle the influx of patient data and that new solutions integrate with existing digital environments. With proper planning and embracing the latest digital technologies, healthcare can enter a new era of more efficient, precise, and effective patient care.