In This Issue:
- The 5 Reasons Why Every Doctor Should Have a Side Gig
- Securing Spare DEA Registration for Smooth Locum Tenens Assignments
- Experts Share Tips for Physician Contract Negotiation in CompHealth Webinar
- How to Avoid These 3 Common Locum Tenens Mistakes
- Physician Falls to 6th on List of Best Healthcare Jobs
- 10 Ways Physicians Can Save Money on Groceries
- Medscape Survey Reveals Rising Doctor Burnout & Depression
- CME Course Offers Strategies for Combating Physician Burnout and Stress-Related Illness
- 5 Steps Physicians Can Take to Seize Control of Their Mental Health
- Aya Locums Executive Shares Locum Tenens Work is a Viable Solution for Fighting Burnout
- Survey: Burnout Uncommon Among Locum Tenens Physicians
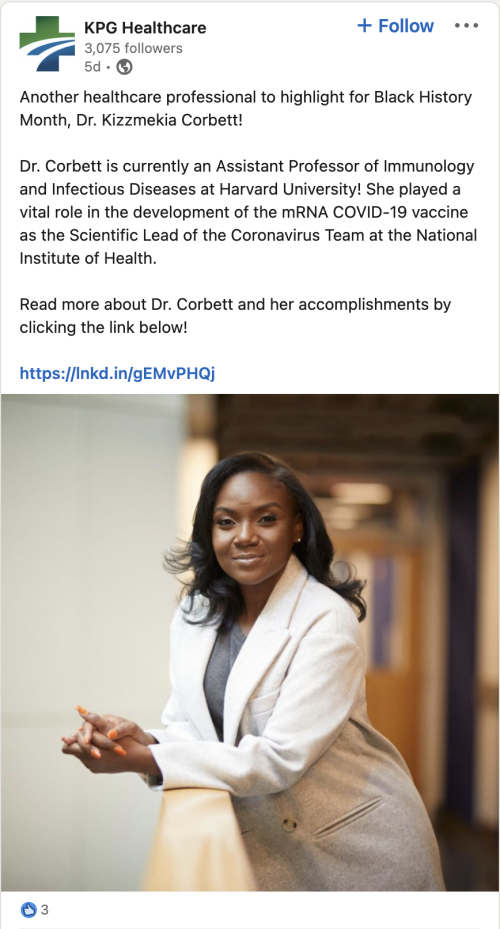
- Socially Speaking: Posts of note from All Star, Hayes Locums, KPG Healthcare, Wapiti, Western, Weatherby, VISTA, RadarHealth & more.
- Machine Learning Model Predicts Physician Turnover
- Study: Primary Care Doctors Offering Mental Health Services May Alter Practice Structure
The 5 Reasons Why Every Doctor should have a Side Gig
(From KevinMD.com, 1/28/23)
Why is it that physicians are seeking alternative avenues to boost their income? It may seem counterintuitive for busy clinical doctors to pursue a side gig, why? In a post-pandemic era, physicians are plagued by colossal debt and increasing rates of burnout. More than 100,000 physicians have left the profession since the start of the COVID-19 pandemic. My peers are frustrated, tired, and seeking a way out. For many, side gig income offers them an exit ramp.
Here are the five reasons doctors should have a side gig.
1. Diversifying your income portfolio
Most entrepreneurs (I suspect) would agree that diversifying your cash flow is a good thing. Though doctors’ incomes are their financial superpower, it also allows them to invest their money in other means of income generation.
Enter the side gig. Side gigs (or side hustles) are an individual’s business pursuits to create a revenue stream in addition to their primary profession. For example, I have started blogging and writing as The Motivated M.D. I hope to utilize the platform I have created to interact with peers with similar financial struggles while monetizing the website. For others, side gigs may include podcasting, creating online courses, real estate investing, and many more. These hustles are not always lucrative, but they provide a means for doctors not to be reliant on their medical careers to maintain their lifestyles.
2. Financial security
Financial security may seem guaranteed in healthcare professions … but nothing is certain. It is appropriate to assume that individuals will always have health concerns. With advances in modern medicine, those individuals are living longer while accumulating more comorbidities. As a result, each subsequent patient cared for is generally older and more complicated. Continuing to place more stress on an already burdened healthcare system.
If doctors can generate income through dividend investing, the creation of digital products, or real estate, this offers a monetary pathway to offset their clinical burden. Maybe they don’t pick up that extra shift? Perhaps they don’t need to be on call so much. The income afforded through a profitable side hustle can cultivate opportunities that contractual negotiation often cannot.
3. Expediting financial independence
As I alluded to, doctors are often delayed in building their retirement savings. While it is true that physicians are salaried while in residency training, reimbursement is commonly well below the U.S. median household income based on 2021 census data. Therefore, once doctors complete their training, they are behind their non-physician peers regarding retirement savings.
Side gigs for physicians create pathways for doctors to “catch up.” Side gig income generation is variable, but the ability to see your net worth improve faster than it otherwise would is relieving. This can be especially true for those exiting training with educational debt. Moreover, a subset of the physician population wishes to go a step further, reaching financial independence and retiring early. This is often referred to as the FIRE movement.
4. Live like a resident
For doctors, there are a few ways to expedite FIRE. One is to live drastically below their means. This can mean saving 50 percent or more of your annual income. “Live like a resident,” it is often called. Treat your expenses as if you are still in training for 5 to 10 years following the completion of your education. This is one way you can expedite financial freedom. This strategy is simple, but it is not easy. It can be financially, mentally, and emotionally challenging to ask an individual who has delayed their income potential for decades to restrict their quality of life for another decade.
Another avenue is the creation of a business. For doctors with the time, grit, and initial capital, a side gig can evolve into a business that generates revenue in tandem with their medical careers. It can also offer an outlet for those plagued by burnout.
5. Preventing burnout
As mentioned above, the global pandemic has placed immense strain on an already stressed health care system. Individuals across all positions in the medical community have felt this pressure. It has led to a mass exodus from the profession, which is not limited to the medical profession alone.
Though altruism is critical to careers in health care, it can be a finite resource. Rely too heavily on the altruism of others, and you risk extinguishing the fire that invigorates their calling. Burnout is quickly becoming the most pressing crises in modern health care professions. Generating other streams of income is not the fix that our health care system needs, but for many individuals, it offers an outlet when their profession asks too much of them.
Your Locums Prescription
(From The Locum Tenens Guy, 1/31/2023)
A recent e-newsletter from The Locum Tenens Guy explained that one of the most common reasons for not starting a locums gig on time is the lack of a spare DEA registration. This is a common thing doctors overlook when working locums.
To work a locums assignment, the provider must have at least two DEA registrations, one for your primary state and another for any state you may be working in. Having a spare DEA registration allows you to quickly transfer it to another state, saving time and hassle.
It is important to note that you may need more than two DEA registrations if you work in multiple states. For example, you would need three DEA registrations if you work one week in Pennsylvania, the next week in New York, the third week in Maryland, and so on.
Don’t let a lack of a spare DEA registration hinder your locum tenens career. Be proactive and secure your second (or third) DEA registration to avoid any future delays in your credentialing process.
(Written based on CompHealth’s Webinar, 2/9/2023)
CompHealth recently hosted a webinar on the topic of negotiating physician contracts effectively. The expert panel consisted of Jon Appino, CEO and Director of Physician Education at Contract Diagnostics, Kim Stranger, a Partner at Holland & Hart LLC, and Dr. Kathryn Sarnoski, Director of Physician Education at Contract Diagnostics. Michael Atkinson, Vice President of CompHealth’s Permanent Placement Division, moderated the discussion.
The panel delved into the various aspects of contract negotiation, providing advice on what to look for in a contract, what items are typically negotiable, and how to communicate what a physician wants effectively. This information can be important for physicians who are or want to do locum tenens assignments and physicians in permanent positions.
The panelists stressed the importance of conducting thorough due diligence before signing a contract, including researching the employer, talking to other physicians, and understanding all aspects of the contract, not just compensation.
Common mistakes physicians make during contract negotiation include not taking enough time to examine the contract, not considering all aspects beyond compensation, and needing to understand termination clauses. The panel provided tips for effective negotiation, including staying calm, asking questions, and having data to support their case. They emphasized the importance of understanding the story behind the opportunity, total compensation, and regulatory limits.
For more information on physician contract negotiation, you can watch and read the entire transcript of the webinar here.
(From MPLT Healthcare, 1/17/2022)
In a blog post, MPLT Healthcare outlined the three common mistakes locum tenens should avoid as they take on their next assignment.
1. No Malpractice Insurance.
With every locum tenens assignment, it’s vital to have a malpractice insurance plan in place in case you’re faced with a lawsuit. Many locum tenens agencies will include malpractice insurance as a benefit of working for the agency, making it a seamless process. However, if you choose to take an assignment on your own, ask the facility if malpractice insurance is provided.
2. Lack Of Adequate Skills And Experience.
Before accepting your first locum tenens job, confirm that you have the appropriate training and credentials to perform the assignment. Reviewing the job’s requirements and responsibilities – and assessing how your qualifications match up – will ensure that you’ll be able to meet the healthcare facility’s expectations and contribute to their team in a productive and safe way.
3. Poor Attitude.
While not every locum tenens job will be a perfect experience, your attitude and perspective can often make or break your performance as a locum tenens provider. Going into every assignment with an open mind and a willingness to learn will make a positive impression on patients and colleagues alike, building your reputation in the field.
Avoiding these common pitfalls can lead to a successful long-term locum tenens career and greater fulfillment and job satisfaction as a healthcare provider.
(From Becker’s ASC Review, 2/1/2022)
Physician dropped to the sixth-best healthcare job, with a median salary of $208,000 and 19,400 projected jobs between 2021 and 2031, according to a U.S. News & World Report list. The role was ranked fourth by U.S. News & World Report in 2022.
For its analysis, U.S. News staff identified jobs with the largest number and percentage of projected openings from 2021 to 2031, according to data from the Bureau of Labor Statistics. Then, each career was assigned a weighted average score out of 10 based on the following component factors: median salary, unemployment rate, 10-year growth volume, 10-year growth percentage, future job prospects, stress level, and work-life balance.
U.S. News also released a list of the 100 best jobs for 2023. Here are the 11 healthcare jobs that made the top 25, accompanied by their rank:
2. Nurse practitioner
3. Medical and health services manager
4. Physician assistant
6. Physical therapist
10. Dentist
13. Physician
14. Orthodontist
17. Registered nurse
19. Occupational therapy assistant
24. Oral and maxillofacial surgeon
25. Nurse anesthetist
(From White Coat Investor, 2/4/2023)
The White Coat Investor recommends the following ways to save money on groceries.
1. Choose where you shop carefully, as certain stores are generally more expensive than others. Walmart and Aldi are usually the lowest-cost providers of non-bulk nonperishables. Trader Joe’s and Whole Foods are more expensive and should be used as specialty stores.
2. Consider going local for produce and perishables. Purchasing items at a nearby farmers market or farm share can be cheaper than buying them at big box stores. Just like in cooking, finding all the right ingredients – such as the correct diagnosis and treatment in medicine – can improve a patient’s health. Learn from a doctor how medicine and cooking can work together to treat a patient’s health.
3. Eat in-season produce to avoid inflated costs due to shipping.
4. Consider bulk buying staple nonperishables from stores like Sam’s and Costco to save money per unit. Consider these 10 frugal hacks to save money automatically when buying your groceries in bulk.
5. Consider couponing and credit card offers to take advantage of cash-back offers at certain stores.
6. Shop online for groceries to avoid impulse buys and to watch delivery costs.
7. Shop at ethnic stores for cheaper spices, produce, and meats.
8. Save money on alcohol by researching and comparing prices carefully and looking for deals like coupons and cash-back offers. Learn more by checking out Real-Life Examples of Physician Budgets — From the Frugal to the Extravagant.
9. Batch cook and make things from scratch to save money on food. You can make many things at home that you might have thought you needed to buy pre-packaged.
10. Avoid shopping while hungry to prevent impulse buying and overspending. Implement grocery hacks like shopping for nonperishables at discount stores and perishables at local stores to save money on groceries over time.
Physician Wellness Retreat
(From Fierce Healthcare, 1/30/2023)
Physician burnout and depression continue to worsen, according to a new report from Medscape. The findings are especially concerning at a time of waning COVID-19 and greater awareness of the harmful effects of physician burnout and depression, Leslie Kane, senior director of Medscape Business of Medicine, told Fierce Healthcare.
“You might think that maybe things are getting a little bit better, but they’re definitely not,” Kane said.
In the survey, more than half of physicians said they are feeling burned out, up from 42% saying so in 2018 and 47% in 2021. Nearly a quarter also reported being depressed in 2022. Most said job burnout was the reason for their depression, with nearly half also saying world events significantly contributed to it.
The “I Cry and No One Cares” report is based on a 2022 Medscape survey that reached more than 9,100 U.S. physicians across 29 specialties. The report is so titled after the confession of a respondent in the survey.
Emergency medicine continues to be the medical specialty experiencing the highest levels of burnout, per the survey, followed by internal medicine and pediatrics. The specialties most affected have shifted; the number of emergency medicine doctors, family physicians, and internists experiencing burnout is up compared to five years ago. Women continue to be disproportionately impacted by burnout. Two-thirds of doctors said burnout has negatively impacted their relationships.
This year’s report showed less burnout in solo practices than in other work settings, thanks to greater autonomy and control over productivity. Kane suggested that some doctors might consider switching their form of practice to help reduce burnout.
For most doctors, workplace stress is caused by too many bureaucratic tasks like paperwork, lack of respect from co-workers, long work hours, and insufficient compensation. There are some tactical tools that can help, but not solve, the problem, Kane suggested, like using a scribe for note-taking or leaning on artificial intelligence to fill out prior authorization paperwork.
Most cope with burnout by exercising and talking with family or friends. Nearly a third have reduced work hours.
What would help most with burnout, doctors reported, is higher compensation, a more manageable work schedule, and more support staff. As more physicians become employed by health systems, the report suggested that they work longer hours than they are paid for. Their only option is to ask for a raise “to at least make them feel more respected and valued,” Peter Yellowlees, M.D., chief wellness officer at the University of California, Davis, said in the report.
Half of the doctors said they believed a union would help combat burnout. But, the report cautioned, that could be a last-ditch effort to bring more attention to the issue. Nearly half of the respondents said their workplace offers a program to reduce burnout, while more than a third said it does not.
Many of these doctors are reluctant to seek professional help for burnout due to the stigma around mental health support. Almost half of the surveyed doctors haven’t sought help, and over a third wouldn’t seek it or tell others about their depression. The survey found that a quarter of doctors are depressed, with two-thirds having colloquial depression, which is feeling down and sad but not meeting the criteria for being clinically depressed. Furthermore, depression leads almost a fifth of doctors to be less careful with patient notes and nearly a third to become easily exasperated. Peer groups and mental health support programs for doctors are crucial to address these issues. Keeping communication with provider organization leadership is key to preventing doctors from leaving the profession over burnout.
Kane encourages doctors to try small changes: “The big thing is to try,” she said. “Whatever you can, little things can make a difference.”
(From Pulmonology Advisor, 2/4/2023)
A survey of US physicians and advanced practice clinicians highlighted in a Pulmonology Advisor article found a significant increase in burnout and intent to leave medicine from 2019 to late 2021, further contributing to the projected physician shortage in the US due to a “broken healthcare system.” To address this issue, Dr. Robyn Tiger, a radiologist and founder of StressFreeMD, developed the CME-accredited course Rx Inner Peace: A Physician’s Guide for Self-Care, which teaches self-care strategies for physicians to help prevent burnout and promote resilience in the face of stress, anxiety, depression, and burnout. Additionally, Dr. Tiger is collaborating with the American College of Lifestyle Medicine and various medical societies to promote stress management and self-care for physicians.
The need for such programs is becoming increasingly apparent as physician burnout remains a pressing concern. If current trends continue, up to 47% of healthcare professionals may have left the profession by 2025. Programs such as Rx Inner Peace offer a way for physicians to combat burnout and promote self-care, which can help to alleviate the projected physician shortage in the coming years. However, whether such efforts will be enough to address the structural issues within the healthcare system that contribute to physician burnout and attrition remains to be seen.
In an in-depth interview with Dr. Tiger, learn more about what physicians can do to address stress and burnout.
(From Medical Economics, 1/24/23)
In a Medical Economics news article, Noah Nordheimer, CEO of All Points North, discussed the company’s provision of whole-person health treatment for behavioral, mental, and physical well-being. Nordheimer highlights the problem of physician burnout, particularly in the wake of the COVID-19 pandemic and the stigma preventing doctors from seeking treatment for their mental health.
Here are five concrete steps healthcare workers can take to improve their wellness:
1. Remember healthcare workers are human too.
Healthcare workers are not invincible and need rest, recovery, and care like everyone else. Prioritizing patient health is important, but neglecting their mental and physical well-being can lead to burnout, trauma, and exhaustion. To provide quality care, healthcare workers must take care of themselves.
2. Mental health is essential to overall health.
Mental health care is just as critical as physical health care. Treating anxiety, depression, or burnout is crucial to overall well-being. Seeking support for mental health is not something to be ashamed of.
3. Find a personalized healthcare provider.
Healthcare workers should find a provider who addresses their unique needs through customized treatment, not a one-size-fits-all approach. For those experiencing depression, anxiety, or PTSD, consider therapies like EMDR, ketamine-assisted therapy, or Deep TMS.
4. Access helpful resources.
Demand better resources by accessing Physicians Health Programs through the Federation of State Physician Health Programs. Your internal healthcare management should prioritize clear communication and provide internal support programs.
5. Consider telehealth options.
In-person therapy can be challenging to schedule, but telehealth options like mental health apps and group telehealth sessions can provide support when needed. This crisis highlights the need for change and confronting mental health stigma.
(From Medical Economics, 2/10/2023)
Sophia Morris, executive vice president at Aya Locums, wrote in a Medical Economics article that locum tenens work is a viable solution for physician burnout. Locum tenens offers physicians a way to fill in for absent colleagues, and it also provides a flexible and sustainable way to address burnout. Taking a locums assignment also offers freedom, financial benefits, and the opportunity to gain diverse experience, build a network and explore new career paths.
Morris also mentioned the benefits of taking locum tenens assignments could reduce administrative burdens as physicians typically won’t have to handle day-to-day operations as they would in a permanent position. Furthermore, locums offer an opportunity to travel and work in various locations, which can help alleviate boredom and dissatisfaction from a monotonous, low-travel lifestyle. Most assignments cover travel and accommodation expenses, making it a great option to see new places while combating burnout.
To combat burnout, Morris emphasizes the need to reflect on the sources of stress in one’s life. If someone is burnt out and seeking a change, they may find locum tenens work to be a viable solution.
This work offers freedom, flexibility, and financial benefits, as locum tenens physicians earn 20% more than employed physicians. Moreover, it is an excellent way to shake up a career, gain diverse experience, build a network, and explore new career paths.
(From Urology Times, 2/7/23)
In a Urology Times news article, a recent survey of 2,500 clinicians found that burnout is a rare occurrence among locum tenens physicians. While 40% of doctors in permanent jobs experience burnout, only 29% of locum tenens contractors experience the same.
Physicians are becoming increasingly dissatisfied with their current positions, with at least 61% likely to look for a new role within the next year and 27% of those wanting to leave, citing general dissatisfaction with their current position. This dissatisfaction is particularly true of younger physicians, with 21% under the age of 40 reporting as currently not practicing.
Locum tenens is an attractive option for physicians. The study found that 73% of physicians who don’t currently work on a temporary basis would prefer to work locally, 63% would be willing to work jobs that require travel, and 55% would be interested in working more hours via telehealth. This trend could be attributed to a shift in physician perception of locum tenens work. According to the survey, 96% of peers value the contributions of locum tenens clinicians.
Chris Franklin, the president of LocumTenens.com, stated that organizations that embrace flexible models like locum tenens and utilize technology solutions would be able to attract more talent, improve clinician satisfaction, and subsequently improve healthcare outcomes. The rise of the gig economy requires adaptation and transformation of workforce planning and management. The healthcare landscape is shifting, and physicians are embracing it to create a better quality of life for themselves.
Doctor’s Notes
(Edited from YaleNews, 2/1/2022)
In a recent Yale University study, researchers used machine learning from electronic health records (EHRs) over a 3-year period to determine the factors that increase the risk of physician turnover. The study published in PLOS ONE found that factors such as the length of a physician’s tenure, age, and case complexity can predict physician departure with 97% accuracy. The study provides insights to help healthcare systems to reduce physician turnover.
The study analyzed information from the EHRs of 319 physicians over a 34-month period from 2018-2021 (including pre-pandemic and pandemic times). The researchers identified four key factors contributing to departure risk: length of employment, age, the complexity of cases, and demand for services. The researchers also found that the risk of leaving was highest for physicians recently hired or with a long tenure, while those with a moderate length of employment had a lower risk. These findings are useful for identifying the factors that lead to physician departure.
The risk of doctors leaving their jobs changed during the study period due to the pandemic. The researchers also discovered specific factors that played a role in a doctor’s decision to leave, such as the number of electronic health record messages responded to by someone other than the doctor, the demand for the doctor’s services, and the number of patients seen. Additionally, the risk of departure was affected by COVID-19 outbreaks.
To help healthcare leaders better utilize this information, the researchers created a dashboard to display this information. As physician burnout is an increasingly recognized problem, healthcare systems, hospitals, and large groups need to figure out what they need to do to ensure the emotional and physical health and well-being of the physicians and other clinicians who do the actual caring for patients.
The findings of this study highlight that there is not a one-size-fits-all solution to reducing physician turnover. The researchers hope their findings will help create a sustainable and thriving work habitat for clinicians, and their dashboard can help healthcare leaders make data-driven decisions. Researchers continue to work on ethical implementation to foster physician well-being and a thriving workforce.
(From Medical Economics, 2/8/2023)
In a Medical Economics article, a new study reveals that more patients receive mental health counseling from their primary care physicians, suggesting a trend that may affect the organizational structure of primary care practices.
The study, “Adult Primary Care Physician Visits Increasingly Address Mental Health Concerns,” analyzed data from the 2006-2018 National Ambulatory Medical Care surveys, which showed a growth in the number of primary care visits with a mental health concern as a primary diagnosis. This figure grew from 3.4% in 2006-2007 to 6.3% in 2016-18, and the percentage of visits that addressed any kind of mental health concern increased from 10.7% to 15.9%, indicating an almost 50% increase during the same period.
The study also found that patients are more likely to receive mental health care from their primary care provider than from other providers. However, there were significant race and ethnicity-based differences, with Black and Hispanic patients being 40% less likely than white and non-Hispanic patients to have mental health concerns addressed during a visit.
According to the authors, there are two reasons for this trend: there aren’t enough mental health specialists, and primary care practices are increasingly incorporating mental health care into their services. The authors also emphasize that primary care doctors need resources to address patients’ mental health needs. These resources can include having therapists or psychiatrists available in the same location, longer appointment times, and billing codes and documentation systems allowing doctors to address physical and mental health concerns.
The findings suggest the need for more mental health resources in primary care settings, particularly in the case of underserved communities. This could boost support for value-based care models and lead to changes in the organizational structure of primary care practices.