In This Issue:
- America Trains Enough Doctors: Redefining Medical Supply and Demand
- 7 Ways You Make an Impact as a Locum Tenens Provider
- Trauma Surgeon Beats Burnout
- Faster Licensing in 32 States And Territories with the Interstate Medical Licensure Compact
- Healthcare Jobs Rebounding, but COVID-19’s Effects Will Linger for Years
- The Trends Physicians Fear Most: 4 Perspectives
- Why This Florida Orthopedic Surgeon Retired Early
- Medical Economics PHYSICIAN BOOTCAMP
- Marketing Tips for Your Medical Practice
- Amazon, CVS Health Look to Primary Care Amid Increasing Healthcare Consolidation
Our Top Story: America Trains Enough Doctors — Redefining Medical Supply and Demand
(Edited from KevinMD post by dermatology practice co-founder Rushi Negalla)
If the US medical system is a chessboard, and providers are the game pieces, America is playing those pieces with one column, row, and role instead of using the whole space.
Several journals, economists and medical professionals forecast physician supply to be dangerously low in 10- to 20-plus years. They’re 100% correct that supply won’t meet demand (as things stand now), but the reasons are flawed.
Alarmists have been complaining about doctor shortages for decades. Physician retirement and burnout don’t explain predicted gaps. The physician shortage everyone worries about is not a lack of new graduates but a grand misallocation of resources.
[Editor’s Note: While the debate continues–and until physician supply is increased or reallocated rather dramatically–the outlook for the locum tenens industry remains bright.]
The Numbers Don’t Tell All
In terms of raw supply, there are just over one million licensed physicians. According to a Federation of State Medical Boards census, the number of doctors grew by 20% from 2010 to 2020. Most of that growth (+168K physicians) is from new graduates.
In the same period, the US population rose ~7% to ~330M. The seemingly reassuring headline numbers are misleading.
Younger millennial doctors are seeking work-life balance; late-career doctors and burned-out providers put in fewer hours at the clinic. The number of doctors aged 60+ grew by 48%, while those aged 49 and younger grew by 16%.
In terms of fresh supply, the number of medical school graduates rose by 32% between 2011 to 2021, but in absolute terms, there were ~28K grads last year. The US population is a slow-growing mega-fountain, while medical providers are a fast-flowing sink faucet. It’s not practical to expect both to balance each other without help.
Shortage and Supply Aren’t the Same
More data gathered by the Kaiser Family Foundation indicate that one primary care doctor serves 665 people on average, while one specialist serves 584 people. The doctor-to-patient ratios appear extremely low in a vacuum, but most physicians can handle patient groups in the low thousands. There’s a critical difference between real capacity and max capacity.
If the US population doubled tomorrow, one average PCP could oversee ~1,300 patients, and one specialist ~1,100 patients. So why do both patients and economists keep worrying about doctor capacity? The answer: Shortage isn’t the same as supply.
Physicians don’t magically pop into clinics, see patients, and then poof away. Amazon.com is better at delivering packages anywhere in two days than we are at having doctors in the right place at the right time.
Hyper-urbanized regions have too many doctors chasing relatively concentrated patient populations. Meanwhile, rural areas have too few doctors to care for smaller numbers of patients who are more widely dispersed.
Most physicians in private and public settings practice during the traditional workweek, some limiting their patient appointments to just a few weekdays. Physicians have to do paperwork alongside patient care.
Even if physicians make themselves available to see thousands of people each, those doctors may still reject Medicare and Medicaid patients because such plans typically reimburse at much lower rates than private insurers do.
To remedy some of these healthcare-delivery woes, our physician supply needs to be realigned instead of rebuilt.
Realign, Rather Than Rebuild
Expanding AI office solutions, targeting more patient demographics by redefining “availability,” and carefully expanding the non-physician workforce (e.g., nurse practitioners and physician assistants) can maximize each doctor’s max patient panel enough to keep up with demand.
Fine-tuning office-visit timing while embracing technology and easing administrative hassles (i.e., vertically integrated disease/drug literature banks, chart notes, insurance claims, and payment systems) are the most appropriate supply-side adjustments. Offering additional time over weekends or after normal business makes care accessible to patients in certain demographies.
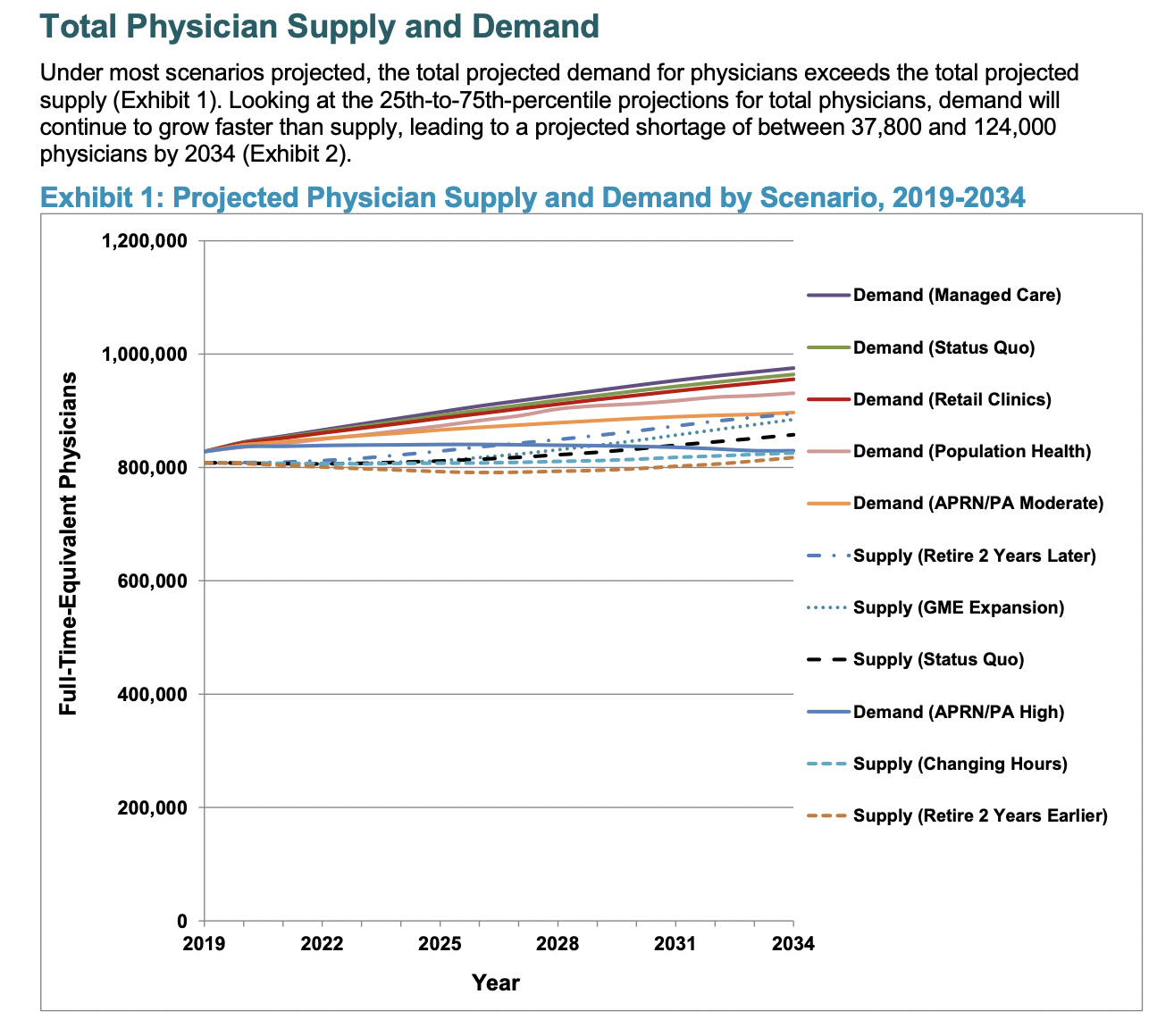
Supply must reach demand somewhere. Our country’s true medical care needs create the shortage in the first place. The Association of American Medical Colleges, or AAMC, publishes a 25-year forecast of physician supply. In their 2019 to 2034 review, the authors calculated demand based on demographic changes, the incidence of diseases affecting the related demographics, and care delivery setting.
Current U.S. medical needs suggest a lack of ~38K to 124K physicians and ~18K to 48K primary care doctors by 2034. Those are massive gaps compared to ~28K expected new medical graduates in 2021, but the AAMC lowered both top ends of those ranges by 12 to 14% year-over-year from their last report. The report highlights four nationwide scenarios for improving real medical capacity (and reducing shortage forecasts).
Total Physician Supply and Demand
Source: AAMC’s The Complexities of Physician Supply and Demand Report June 2021
Stretching Supply is Easier Than Reducing Demand
The first interesting, but impractical, shift to ease demand would have all covered patients join an HMO or ACO insurance network. In this world, medicine, doctors and money are vertically integrated like a company that owns its whole supply chain.
Unending political gridlock precedes this outcome based on current US healthcare policy and current insurance and physician trade group positioning.
The second demand scenario involves magical thinking, but remains a helpful reference point. The AAMC modeled what might happen if we all lost weight, cut glucose, quit smoking, and reduced cholesterol. Population-wide health improvements prevent shortfalls–but we’re human.
The next two possible futures in extending supply appear somewhat reasonable.
Thinking More Realistically
First, drugstore chains like CVS and Walgreens are sprouting more and more clinics. The proliferation of these retail clinics introduces alternative primary care facilities treating minor, but acute, issues. It’s efficient for patients to get basic goods, prescriptions, and routine medical exams at the same place. If referrals are necessary, patients can still get those permissions and move on to see specialists rather than wait for advice from traditional medical practices.
Second, adding more registered nurses and physician assistants under strict oversight could help plug gaps of care that doctors can’t easily reach.
Combining all these scenarios might ensure that providers can heal Americans faster while preventing the need to grow doctors on trees.
Whatever the consensus definition for the US physician shortage, cleaning up healthcare delivery, better utilizing retail clinics and advanced practitioners, and redefining availability to target broader patient-demographic segments can reduce the gap between clinician supply and patient demand. Patients who understand this situation will better handle whatever changes occur next to our fragmented healthcare system.
The late Dr. Ken Teufel quoted Harvard Business Review’s advisory board in a “Dr. Ken’s Corner” blog post for Interim Physicians dated June 23, 2020 [speaking about a predicted deficit of primary care physicians that could grow to 55,000 PCPs by 2023]: “It’s time to stop panicking about a looming ‘shortage.’ Rather, the real shortage is one of courage to disrupt the way things have been done for decades.”
All News Is Locums
7 Ways You Make an Impact as a Locum Tenens Provider
(Edited from All Star Healthcare Solutions® blog, 8/10/2022)
Whether you choose locum tenens to supplement your income, to experience a variety of locations and settings, or to transition into a new career stage (from residency to retirement and in between), you make an important impact with each assignment.
1. You extend high-quality care to those in need.
According to McKinsey research, 45% of Americans admit to having at least one unmet healthcare need. Locum tenens professionals help mitigate those circumstances, so individuals can receive the attention they need and deserve. What’s more, because locum tenens providers are not involved with many of the facility’s administrative duties, you have more freedom to hone in on patient interactions.
2. You empower facilities to maintain continuity of care.
Hospitals, clinics, and other healthcare organizations experience fluctuations in patient census, personnel vacancies or family/medical leaves, and other factors that affect staffing needs. Accepting locum tenens jobs not only answers the demand for clinicians, but also helps facilities preserve continuity of care, too. Units are better manned to meet patient demand and sustain services.
3. You provide specialty coverage.
The shortage of primary care physicians has been well documented; however, numerous specialties remain underrepresented. For example, the American Journal of Surgery published a study that indicates nine surgical specialties are in jeopardy of incurring staffing shortages by 2030. Compounding the situation is a concentration of high-acuity specialists choosing to practice in urban centers, which leaves smaller and rural communities at a disadvantage. Whether your locum tenens contracts take you to the country or a city, as a specialist, you make an impact on patients’ care and a facility’s ability to meet the community’s needs.
4. You ease the demand on staff.
As patient needs grow, so does the call for quality clinicians, even though the physician shortage shows no signs of slowing. This confluence of factors creates a dynamic that weighs heavily on a facility’s personnel—namely, larger caseloads and longer hours. According to a pre-COVID survey conducted by The Physicians Foundation, the majority of physicians average between 41 and 60 hours on the job per week. Locum tenens providers help even out duties by assuming a portion of caseloads. Advanced practice providers in temporary positions also shift clinical responsibilities, allowing physicians to concentrate on more critical cases.
5. You share your skills.
As a locum tenens professional, you are invited to observe various practice styles and how cultural and regional aspects influence healthcare. Accumulating that knowledge can enhance your own practice as well as impact fellow practitioners and their patients by sharing the experiences you collect along the locum tenens journey.
6. You support the community.
Your presence can make a noteworthy difference where access to healthcare infrastructure is limited. For example, the Association of American Medical Colleges (AAMC) confirms three out of five federally designated health professional shortage areas exist in rural areas. Fulfilling locum tenens assignments at rural facilities, or within urban healthcare deserts, expands care for patients but supports the facility’s role in the greater community, too. Hospitals typically operate as a major employer in town and contribute to the local economy. So, even temporarily, your contribution leaves a larger impact on the community in addition to treating individuals.
7. You become a friend.
Yet another impactful impression locum tenens professionals make is with their friendship, forming enduring relationships with co-workers you meet on each opportunity.
Trauma Surgeon Beats Burnout
(Edited from “The Art of Medicine” blog post by Dr. Andrew Wilner, 8/21/2022)
In this episode of “The Art of Medicine with Dr. Andrew Wilner,” a trauma surgeon talks about how locum tenens allowed her to continue practicing medicine after quitting her full-time job with a severe case of burnout.
Following her residency, Dr. Serene Shereef struggled with balancing three children, a husband, and the demanding life of a trauma surgeon. She tried both academic medicine and community practice, but was miserable.
Finally, with the help of a couple of coaches and a reassessment of her life’s priorities, she found a part-time position that allows her to practice surgery while offering quality time for her family and other interests. She says she’s happier than she’s ever been and eager to share her advice with other physicians wrestling with work/life balance.
You can watch this interview on YouTube: http://www.youtube.com/c/andrewwilnermdauthor
Dr. Shereef has a podcast, “Mindfulness and Productivity Systems Podcast.” (The title says it all!) You can reach Dr. Shereef on her social media channels.
Faster Licensing in 32 States And Territories with the Interstate Medical Licensure Compact
(Edited from Global Medical Staffing Blog post by Kari Redfield, 7/13/2022)
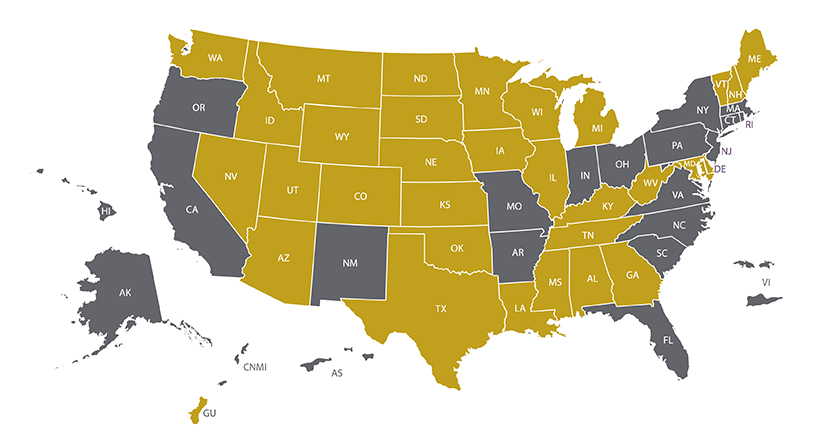
Physicians can now get expedited licensure to practice medicine in most US states. The Interstate Medical Licensure Compact (IMLC) allows medical doctors to move quickly through the licensure process in 31 states and the territory of Guam.
This is a boon for physicians interested in working locum tenens. Interested in working in Guam so you can enjoy the tropical climes and experience a new culture? Great! You can get started much more quickly. Want to escape the winter blues for some weekend shifts in sunny Texas? Awesome. Let’s get you lined up.
Getting licensed in additional states is simpler with the ever-expanding number of IMLC-member states. And the IMLC process reduces the time to get a new license from months to just weeks in many cases.
How It Works
As the IMLC explains, eligible doctors complete a single application and then receive separate licenses from each state in which they intend to practice.
As usual, the license is issued by each individual state, but because the application goes through the IMLC the overall process is streamlined. That means that you can get licensed to practice in more states faster and with less work.
So how do you qualify and apply? And how long does it take? Keep reading.
Rather see this all through a video? Watch a general overview here.
How You Qualify
First, you need to declare your “State of Principal License” (SPL), where you hold a full and unrestricted medical license. To designate your SPL, you must complete an application and then receive a formal Letter of Qualification from that state. Then the SPL shares this information with the additional states where you want to practice.
The Interstate Medical Licensure Commission explains the qualifications that are required to apply for a license. At least one of the following must apply:
- Your primary residence is in the SPL.
- At least 25% of your practice of medicine occurs in the SPL.
- You’re employed to practice medicine by a person, business or organization located in the SPL.
- You use the SPL as your state of residence for US federal income tax purposes.
And, of course, you must be in good standing without a criminal history, have no disciplinary actions against your medical license, or be under investigation.
[Watch a video about qualifying for the IMLC here.]
You must:
- Have graduated from an accredited medical school, or a school listed in the International Medical Education Directory.
- Have successfully completed ACGME- or AOA-accredited graduate medical education.
- Passed each component of the USMLE, COMLEX-USA, or equivalent in no more than three attempts for each component.
- Hold a current specialty certification or time-unlimited certification by an ABMS or AOABOS board.
Following these standards, about 80% of US physicians already meet the criteria for licensure through the Compact.
States and Territories that Offer Expedited Licensure
(IMLC-member states map as of March 2022):
Many states have elected to join the IMLC voluntarily to help address the physician shortage. To participate, a state’s legislature introduces and enacts a bill authorizing the state to join. Current IMLC member states and territories include:
Alabama
Arizona
Colorado
Delaware
Georgia
Guam
Idaho
Illinois
Iowa
Kansas
Kentucky
Louisiana
Maine
Maryland
Michigan
Minnesota
Mississippi
Montana
Nebraska
Nevada
New Hampshire
North Dakota
Oklahoma*
South Dakota
Tennessee
Texas
Utah
Vermont*
Washington
West Virginia
Wisconsin
Wyoming
*Oklahoma and Vermont are not current “States of Principal Licensure”, which means you are able to get a license issued for these states through the compact if you qualify through another SPL but neither state qualifies as a SPL for licensing in other states.
States Working on Getting Expedited Licensure Up and Running
The following have joined the compact but are awaiting full implementation:
- Connecticut
- New Jersey
- Indiana
- Ohio
- Pennsylvania
- Washington, DC
States with pending legislation to join the compact include:
- Massachusetts
- North Carolina
- Rhode Island
So, for physicians interested in working locum tenens, the IMLC significantly simplifies and speeds up the licensing process to take locum assignments in more areas of the nation.
To learn more about getting licensed through the IMLC, watch additional videos from the IMLC. Or check out The Locums Guy’s guide to the IMLC for a locum physician’s perspective.
The Healthcare Staffing Story
Healthcare Jobs Rebounding, but COVID-19’s Effects Will Linger for Years
(Edited from Medical Economics article by Richard Payerchin, 8/26/2022)
“Relatively recession-proof” sector tanked in spring 2020, but not as badly as overall economy, report says.
Healthcare jobs largely have rebounded to pre-pandemic levels, although COVID-19 will affect healthcare and the entire US job market for years to come.
The Peterson Center on Healthcare and KFF’s Health System Tracker compiled and analyzed employment figures from the US Bureau of Labor Statistics’ Current Employment Survey (CES) and the Job Openings and Labor Turnover Survey. While the pandemic recession may be over, “recovery is incomplete,” said the report entitled, “What Impact Has the Coronavirus Pandemic Had on Health Employment?” published this month.
July 2022 was the first month since the pandemic that non-health-sector jobs rose above February 2020 levels, the report said. Even with gains, healthcare sector employment was 0.5% lower than in February 2020.
Health Sector Bounces Back Faster
According to the report, “By July 2022, physicians’ offices, outpatient care centers and home health services employed more people than they had in February 2020, and hospitals were within 2% of their pre-pandemic employment level. However, employment in these industries is still below expected levels, given pre-pandemic trends.”
Healthcare employment has “been relatively recession-proof,” nudging upward even during the “Great Recession” of December 2007 to June 2009. It tanked with the rest of the economy in spring 2020, falling from total health employment of 16.5 million people in February 2020 to 14.9 million two months later.
Measuring year on year, that was not as bad as the rest of the job market. Health employment fell 8.3% from April 2019 to April 2020, while nonhealth-care-related employment dropped 13%, the report said.
Within healthcare, physicians’ offices had a drop in workers of about 11% in April 2020, but they have rebounded most strongly, reaching pre-pandemic levels in about April 2021 and now showing about 4% growth.
COVID-19 Threw Projections Off
Every area within the healthcare sector, except for nursing care facilities, were growing steadily before March 2020. But even with recent gains, no areas of the health care sector have reached levels of job gains that were projected before COVID-19, based on pre-pandemic rates.
For example, in-home health jobs grew by 0.28% per month from 2017 to early 2020. Had that continued, home health service workers would number 1.68 million in July 2022, instead of 1.57 million, the report said.
The pandemic’s effect on healthcare employment was smallest for physicians’ offices, where the July 2022 employment was just 0.8% below projected growth levels from before the pandemic. The decline in employment was most pronounced for nursing care facilities (-12%) and community care facilities for the elderly (-13.5%), according to the report.
The Trends Physicians Fear Most: 4 Perspectives
(Edited from Becker’s ASC Review, 8/26/2022)
Healthcare’s ever-changing landscape comes with a host of uncertainties. Here is what four physicians had to say about their fears regarding current healthcare trends:
Editor’s note: These responses have been edited lightly for clarity and brevity.
James Bradley, MD. Orthopedic Surgeon at UPMC: “The devaluing of the physician with extensive clinical experience and wisdom because of increasing administrative burden to treat our patients, thereby causing early burnout, is the biggest danger to our profession today.”
Read the full story here.
Kian Eftekhari, MD. Oculofacial Plastic Surgeon at Eyelid Center of Utah (Salt Lake City): “As an independent physician, I think the biggest threats right now are scope of practice expansion efforts in optometry, nursing and physician assistants, which would allow state legislatures to make medical school, residency training and clinical experience an “unnecessary burden” for anyone who wants to practice medicine and surgery.
“Without appropriate input from physicians about how this will affect patient safety, I worry we will worsen clinical care for future generations, including when I need a doctor one day.”
Read the full story here.
Vikas Patel, MD. Executive Vice Chair of University of Colorado Medicine (Denver): “The biggest threat facing physicians right now is the business of medicine.
“Medical care for physicians has become much more of a business from every aspect, compared with what used to be the ‘art’” of medicine. Physicians are now pressured to see more patients in the clinics and document more irrelevant aspects of the visit, far more than spending time getting to know their patients and understanding their patients’ problems.
“Office procedures, such as injections, add to this, as injections garner more reimbursement than just an office visit, not to mention the ‘ancillaries’ of imaging, physician therapy, etc. All of this pressure comes from decreased reimbursements and a need to cover the ‘overhead’ costs of a practice. So if costs go up, physicians are pressured to increase throughput and find other ways to cover the cost of patient care.
Read the full story here.
Bradley Shapiro, MD. Gastroenterologist at Duly Health and Care (Hoffman Estates, Ill.): “The proposed 4.42 percent pay cut for physicians is appalling and shows lack of appreciation for our profession.
“Soaring inflation results in increased overhead, including labor and supplies, vital to running a medical practice. I anticipate this will lead to closures of smaller medical practices, as they will not be able to absorb the increasing costs amid decreasing revenue.
“Some internal medicine physicians will likely turn to concierge medicine in order to enhance revenue. As Medicare puts the squeeze on physicians, many will retire earlier than expected, decreasing availability for patients.
“More than 43 percent of the physician workforce is 55 and older. These changes will result in physician shortages and decreased access to care for our patients, especially in the primary care setting. I can only hope our medical societies can adequately express these concerns to Congress and amend these proposed changes.”
Read the full story here.
Why This Florida Orthopedic Surgeon Retired Early
(Edited from Becker’s ASC Review, 8/4/2022)
Jonathan Phillips, MD, former orthopedic surgeon at Orlando (Fla.) Health, joined Becker’s to discuss how the potential CMS pay cut will affect patients and why he chose to retire early.
Editor’s note: This interview was edited lightly for clarity and length.
Question: If CMS follows through with its proposed 4.42 percent physician pay cut, how will physicians & patients be affected?
Dr. Jonathan Phillips (JP): I recently retired at the age of 62. There were many reasons, but the most important was a decrease in salary of 10 percent over a two-year period as a result of a contract renegotiation with my employer. A decrease of 4.4 percent by CMS will effectively be a greater than 10 percent salary loss in real terms, given 8 percent inflation.
We only have to look at the recent spike of resignations by senior physicians in the United States to predict what’s going to happen. We are already looking at a shortage of thousands of doctors over the next several years, and this will exacerbate the problem hugely. Access to timely healthcare in the United States will be severely harmed, and patients will suffer. I am one of those patients now, and I’m concerned for the future of my own healthcare.
It’s inconceivable to me that anyone within administration at CMS would accept a 4.4 percent pay cut. It just does not happen. The same goes for hospital administrators who increasingly expect physicians to work longer hours for less money so they can profit from our efforts. There is a parallel in the nursing profession, and we have seen the wave of resignations and retirements there, too.
Q: How will declining physician pay alter the healthcare industry?
JP: Until our government realizes that they have created a hugely toxic environment that healthcare workers increasingly decide not to tolerate, the standard of medicine in this country will continue to decline. The disempowerment, disrespect and interference in clinical practice at all levels in this country is depressing. I trained in the National Health Service in the UK and came to the US a long time ago to escape the government’s stupidity in that land. Sadly, we are going in the same direction in my adopted nation.
Tools to Try/News to Use
Make Time for Medical Economics
PHYSICIAN BOOTCAMP
Beyond the Classroom Business Training for Physicians
Thursday, September 15, 2022
3:00 PM – 7:00 PM EST
Medical Economics® understands it takes more than the things you learned in medical school to run a successful business.
Our fall event is bringing you all new curated resources to help your practice operate more efficiently, while also improving patient care. Our experts will answer any questions you might have about malpractice, membership medicine, remote patient monitoring and EHRs.
Scroll down to see the bootcamp agenda here.
Marketing Tips for Your Medical Practice
(Edited from Dermatology Times article, 8/2/2022)
Harnessing digital marketing tools can help your medical practice grow.
Marketing a practice wasn’t likely part of your medical education, but being able to market yourself is an important part of running any business. Beyond traditional advertising there are other ways you can market your practice and connect with your patients, potential patients, and colleagues.
Boost Your Social Media Presence
You may be on Facebook, LinkedIn, or Instagram, but is your practice? Also, if you have social accounts are you sharing them on your website or advertising them in your practice?
LinkedIn
You can set up a company page that describes your practice; the platform will connect your employees. You ought to at least set up the page, add your logo and basic information. It’s also a great place to share videos, articles or other information for potential patients. Need examples of what to do? Check out WellSpan Health and CommonSpirit Health.
Facebook
You can have a company page on Facebook as well. It’s a great place to share photos of company events, community service, or employee milestones. It allows you to connect with patients and employees in a more casual environment. Also, if you’re looking to bring in new patients, look at Facebook promotion options. You can target your audience and spend as little or as much as you like to reach more people. Check out Multicare Health System and Orlando Health for good examples.
Facebook and most of the other platforms offer options for paid promotion of your posts if you are wanting to target a particular audience.
Instagram and TikTok
If sharing what you do through images and video makes sense, Instagram and TikTok (or other photo and video sharing apps) may be worth spending time on. Instagram and TikTok are usually less formal and may utilize casual videos with helpful information or just be for fun. Check out what OhioHealth is doing on TikTok and Sentara Healthcare and Cleveland Clinic on Instagram.
YouTube
YouTube is great for longer form videos or as a repository for all of your video content. For example, in our business we share physician spotlights on different elements of working locum tenens. Others that have good YouTube pages are Johns Hopkins and PeaceHealth.
Share Your Expertise
As a physician you are an expert in your field. You may have written research papers or submitted to medical journals, but have you looked for other ways to share your expertise?
Company blogs are a great place to share information on what your practice is doing, your latest service offerings, or medical topics that would be relevant to your patients. Sharing that expertise through blogs is another way to bring attention to your practice and establish your credibility. Check out Adventist Health and St. Luke’s for great examples of healthcare-focused blogs.
Not interested in writing a regular blog but still have thoughts you want to share? Many online healthcare publications accept submissions on a variety of clinical and non-clinical topics. Check first with the sites you regularly read and then expand out looking for sites that match the audience you are trying to reach. Also, professional specialty organizations often have opportunities for their members to submit articles, so that is another place to check.
Lisa Grabl is president of CompHealth, the nation’s largest provider of locum tenens physicians and founder of the traveling physician industry.
Healthcare in the Headlines
Amazon, CVS Health Look to Primary Care Amid Increasing Healthcare Consolidation
(Edited from Becker’s ASC Review, 8/26/2022)
Giant companies like Amazon, CVS Health, Walgreens and Walmart are all looking to primary care and physicians amid an increasingly consolidating industry.
Amazon recently announced its plan to acquire primary care provider company One Medical, which could further alter the dynamics of physician recruiting and acquisitions, Forbes reported.
Independent physicians should be prepared for “an entirely new dynamic” when it comes to prospective buyers, the report said. The new market will include unconventional buyers, such as larger retail companies, and there will be a bigger push toward consolidation as more buyers look to buy physician practices.