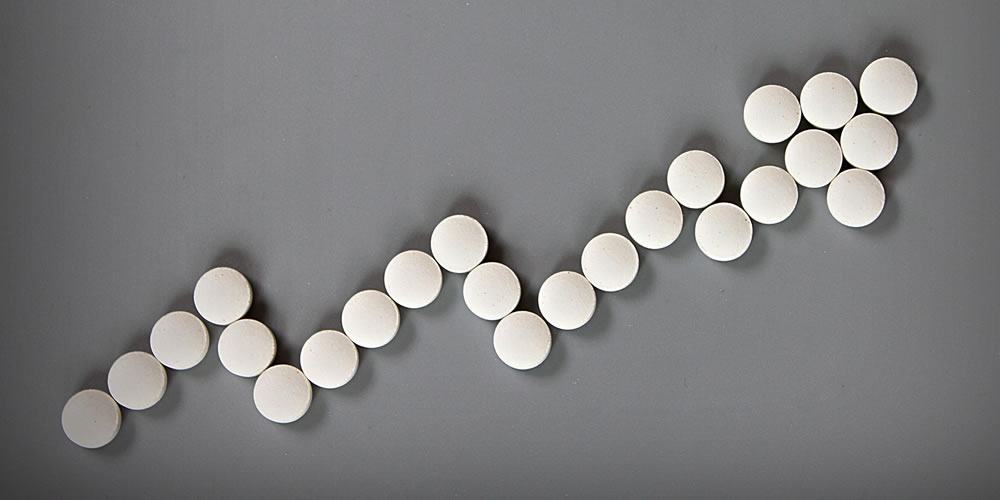
Rising Costs to Slow Hospitals’ Rebuilding Margins to Pre-COVID-19 Levels: Moody’s
Operating cash flow margins for nonprofit hospitals fell to a median of 7% in 2020.
(Edited from Healthcare Finance, 10/26/2021)
A shortage of nurses and other workers will continue to erode hospital financial performance into 2022, according to a new Healthcare Quarterly report from Moody’s.
A rise in COVID-19 “cases (meaning positive test results emanating from often-inaccurate PCR testing)” across the United States has contributed to a wave of often-burned-out nurses’ resigning to take care of family, to work in less acute healthcare settings (such as ambulatory care), or to pursue higher-paying contract opportunities, such as becoming travel nurses.
Hospitals also are challenged to find other types of healthcare workers — such as respiratory therapists, imaging technicians, or nonclinical workers — in areas like dietary, housekeeping, and environmental services.
Why the Report Matters
The report holds no surprises for hospital executives, who already know the financial effect labor shortages are having on revenue. But Moody’s confirms projections that rising costs will make it difficult for hospitals to rebuild margins to pre-COVID-19 levels.
Labor shortages are driving up costs and may be limiting the number of lucrative elective procedures, resulting in lost revenue. Not-for-profit hospitals saw operating cash flow margins fall to a median of 7% in 2020, from 8.3% in the three prior years, according to Moody’s median data.
Hospitals using contract nurses report that hourly wages are very high, in some cases higher now with the Delta variant than during earlier COVID-19 surges. Many hospitals and health systems also have increased minimum wages for nonclinical workers and are finding they must compete with other service sectors, such as the food industry, to attract nonclinical staff.
Given their substantial reliance on government reimbursement from Medicare and Medicaid, most healthcare providers maintain limited pricing flexibility to offset the costs of higher wages.
While there are opportunities for more lucrative commercial insurance contracts, rates are the subject of intense negotiations, limiting providers’ pricing power, Moody’s said.
Providers with strong liquidity (assets easily converted to cash) and diversified cash flow (multiple revenue sources) will remain better positioned to manage stress from cost constraints. Hospitals are taking steps to retain nurses, including developing “float pools” of nurses who can work in multiple departments, increasing retention and merit pay, and expanding healthcare benefits such as mental health and childcare services.
For example, LifeBridge Health, a not-for-profit health system operating in Baltimore and Carroll County, Maryland, paid its nursing staff retention bonuses in December 2020 as the labor market tightened. To recruit nurses, many systems are offering signing bonuses in exchange for multi-year work commitments, as well as scholarship and loan forgiveness programs with local nursing schools.
While these strategies will ease the effect of labor shortages over the long term, they will cause hospitals’ costs to increase in 2022 as salaries and benefits typically represent at least half of a hospital’s expenses. Labor shortages also will likely spark increased unionization efforts or produce more difficult negotiations between unions and providers, potentially increasing costs via new contracts.
The Larger Trend
This Healthcare Quarterly report focused on the impact of labor shortages and cost pressures for various sectors, including hospitals; insurers; pharmaceuticals; healthcare services such as staffing firms; and health insurers.
Health insurers are less affected by labor shortages, wage pressure, and potentially burgeoning inflation than many other healthcare sectors, Moody’s said. Insurers reset premiums each year, which helps them to offset inflation. But if the government does not keep up with payment, providers will look to insurers to make up the shortfall.
Large physician staffing companies, such as Envision Healthcare Corporation and Team Health Holdings, will experience profitability pressure as it becomes harder and more expensive to fill open positions, with clinician burnout and retirements decreasing the number of doctors and nurses available to work.
Travel nurse staffing has higher profit margin resilience compared to physician staffing, the report said.
For real estate investment trusts, worker shortages are slowing net operating income growth for REITs to invest in senior housing and skilled nursing facilities.
Growth in salaries and benefits has exceeded hospitals’ expense growth, a trend likely to continue for the remainder of 2021 and into 2022, Moody’s said in an earlier October report.
One bright spot in the earlier report: Moody’s noted recent increases in nursing school enrollment as indicating a more robust long-term staffing pipeline. However, the aging population, combined with a healthcare workforce that may be retiring from their jobs or quitting due to burnout, represents long-term healthcare staffing challenges nationwide.
All News Is Locums
Comprehensive Guide to Locum Tenens Health Insurance
(Edited from blog post @ The Locum Tenens Guy, 10/29/2021)
Are you switching to locum tenens as a career and looking for health insurance to replace your employer-sponsored plan?
If so, you’d be well-advised to check out The Locum Tenens Guy’s most recent post: Locum Tenens Health Insurance: A Comprehensive Guide.
In his introduction to the subject, ‘The Guy’ commands your attention with a few questions:
- “Who pays for your health and dental insurance when you work locum tenens? YOU.
- “Are any employee benefits included when you work with locum tenens agencies? NOPE.
- “Does it mean that you would need to look for them YOURSELF? HELL YEAH!
Cash “Insurance”
“So…the bad news, it is YOUR job to make sure you’ve got your safety net before switching to full-time locums,” Vladimir Dzhashi, MD, says. “The good news is that this guide is going to give you actionable steps to make this transition as smooth and painless as possible.”
Before he delves into the types and sources of health insurance for locum tenens physicians, he discusses the importance of first creating a cash reserve fund to fall back on when an assignment doesn’t pan out, or when you’d rather not accept the assignment that could see you through a ‘dry spell.’
“You see, cash is your most important locum tenens insurance and the rule of thumb here is to save enough money to cover at least six months of your basic expenses,” Dr. Dzhashi advises. “Having that reserve will not only give a peace of mind if your gigs fall through the cracks but you’ll be in a better position to negotiate with hospitals and locum agencies.”
Health Insurance Options
He then covers the options for maintaining your (and possibly your family’s) health while protecting your wealth from unexpected medical expenses. These options include:
- Securing health insurance through a family member (e.g., spouse or life partner), generally your lowest-cost option.
- Maintaining coverage through your former employer’s health insurance plan under COBRA (not the snake) — generally a costly option.
- Joining a health cost-sharing plan like those offered through Christian Healthcare Ministries, Medi-Share, or Samaritan Ministries.
- Short-term health insurance plans: temporary, year-long, low-premium, and high-deductible insurance policies that may be renewed for up to three years. Typically, these don’t cover things like pre-existing conditions, maternity care, mental health, or prescription drugs.
- Securing private health insurance, through either an insurance broker or your state’s health insurance exchange site (choose state from list)
Private Insurance
“Now if you’re still unsure, just stick to private insurance as it is regulated by the government,” he says. “However, in most situations, costs are high but manageable compared to how much we doctors make.”
Dr. Dzhashi advises this is what most locum tenens docs (including himself) are using. “These plans have no coverage limits or preexisting condition requirements and work similarly to the plan you’ve had as an employee,” he says.
Nevertheless, regarding cost he notes, “The rule of thumb is that your monthly premiums will be at least TWO times MORE and your deductible will be TWO times HIGHER compared to the employer-sponsored plans.
Dr. Dzhashi offers a “decision tree” you can use to make a quick choice.
He wraps up his health insurance guide for locum tenens physicians by covering health savings accounts, dental and vision care coverage, travel health insurance, medical evacuation policies, and the tax deductions a locum tenens physician might take (related to these costs) to lower his or her taxable income for reporting purposes.
Finally, his “comprehensive guide” includes an offer for a free guide to replacing employer-provided benefits like life and disability insurance or retirement planning.
Again, check out “The Locum Tenens Guy’s guide here.
All Star Wins 2021 National Culture Awards
(Edited from Cision/PRNewswire,10/22/2021)
All Star Healthcare Solutions® has earned Energage’s 2021 “Top Workplaces National Culture Excellence” quarterly employer recognition awards in three categories: Employee Well-Being, Professional Development, and Remote Work.
Last quarter All Star earned awards for Compensation and Formal Training.
“Our people are truly remarkable,” All Star CEO Keith Shattuck said. “We have been working remotely for over a year-and-a-half, and our caring, high-performance culture has continued to grow and flourish.”
Energage decides its ‘Top Workplaces’ awards through an anonymous employee engagement survey. “Our employees’ well-being is a top priority, and we are committed to providing them with the professional development they need to be successful,” Shattuck said.
Consilium Staffing Forms New Team to Place Surgical and Subspecialty Locum Tenens Clinicians
(Edited from Cision/PRNewswire, 10/28/2021)
Consilium Staffing announced its formation of a new team dedicated solely to locum tenens placements in surgical and subspecialties, including pulmonary critical care.
While Consilium had been servicing these areas in a lighter capacity before, creating a dedicated team will strengthen its efforts in these specialties and align resources more expeditiously. The team will also focus on placements in obstetrics and gynecology, an area that has seen steady demand even throughout the past year and a half.
Consilium formed this team in response to the changing healthcare environment and to client needs. With surgeries and elective procedures opening up following 2020 lockdowns and accompanying procedural restrictions, the company thinks the time is right for expanding agency resources.
“We’ve seen great stress on the healthcare system, especially in respect to provider burnout, and we wanted to provide more help,” Consilium Division VP and Partner Brent Burrows explained. “This team better positions us to meet our clients’ needs.”
Consilium expects to double the number of team members in this group by the end of this year.
The Healthcare Staffing Story
View From the Boardroom: Improved by COVID
(Reprinted/edited from Staffing Industry Analysts editorial by Jackson Healthcare President Shane Jackson, 10/19/2021)
As staffing company leaders, we likely share a common experience during the pandemic. The past few months may have revealed strengths you didn’t know you and your team had — and maybe some deficits, too.
In my own company, our healthcare staffing, search and technology businesses experienced tsunamis of highs and lows. As hospitals filled with COVID-19 patients, elective surgeries were canceled and patients stopped going to the doctor, creating an imbalance the industry had never seen. Thousands of healthcare workers were furloughed or laid off while hospitals and their partner staffing firms scrambled to find people who could care for critical COVID patients. Healthcare workforce planning flipped to crisis mode with a constant demand for clinical staff to care for drastic patient influxes and to stand in for sick or exhausted clinicians.
We experienced sudden, drastic changes to our business model. To survive (and thrive), we leaned hard into some organizational and operational beliefs that are foundational to the unique workplace culture we’ve built. Here are a few of them.
Working ON or IN the Business. In The 4 Disciplines of Execution, Chris McChesney describes “the whirlwind” of the day-to-day that sucks you in: unending emails, virtual meetings, reports to read. We hate it because it is constant; we love it because we feel accomplished when we check things off the list. That’s working IN the business.
Conversely, working ON the business is strategy. It’s asking, “Are we doing the right things?” versus, “Are we doing things right?” It is making sure that we truly understand the problems we are solving for our customers. It is innovation and improvement. Working ON the business means differentiating and becoming known for that difference. It means ensuring that everyone knows how we define success and how they contribute. It is solving issues before they become problems and ensuring that our associates win when the company wins. During COVID, working ON the business has meant taking a step back to analyze our customers’ problems, assess our core capabilities and create responsive delivery models.
Decentralize Decision-Making. Years ago, we purchased a company out of a distressed situation where the owner was misappropriating company funds. None of the managers had access to the (bogus) financials and as a result, they had no idea what was making money for the business and what wasn’t.
When the leadership received their first set of accurate financials, they lost no time in using them to make a number of changes that transformed their business.
The pace of change during COVID was too great for any one person or centralized group to manage. We were able to quickly respond to our thousands of customers because each individual and team was empowered with the authority and information they needed to respond. All we had to do was get out of their way!
Use Smoke Alarms, Not Fire Alarms. There is only one sound that is worse than that of a smoke alarm in the middle of the night: a fire truck’s siren. Preventing a problem or detecting it early is significantly less costly than fixing one after the fact.
The smoke alarms we have in business — reports, sales funnels, surveys, reviews, and meetings — are all designed to alert leaders when and where there might be a problem while it is still solvable. We were forced into a distributed workforce during the pandemic and, like many, are now contemplating a model with more hybrid options.
Make sure you have alarm systems that provide ways to get insights into how people on your team feel. Employee surveys, meaningful employee feedback and review sessions serve as excellent smoke alarms that can catch a problem before it becomes unsolvable.
Having well-defined organizational beliefs and operational systems can serve you incredibly well in the best of times, and during a crisis, you’ll have the chance to hone those beliefs and systems so they continue to serve you indefinitely.
74% of Companies to Bring in Contract Workers for Holiday Season: Robert Half
(Edited from SIA Daily News, 10/25/2021)
Nearly three-fourths of US healthcare companies (74%) are bringing in contract workers to help with year-end activities, according to a survey released by Robert Half International Inc. (NYSE: RHI).
“This time of year, companies have urgent hiring needs and are tapping contract professionals to help with cyclical projects and spikes in business activity,” Robert Half Senior Executive Director. Paul McDonald said.
The survey included more than 2,800 senior managers in US tech, finance and healthcare companies.
Tools to Try/News to Use
AAPPR Webinar: What It All Means — Interpreting the Latest Annual Benchmarking Report on Physician and Provider Recruitment
(Edited from AAPPR email update, 11/2/2021)
Thursday, November 18, 2021 | 1:00 PM – 2:00 PM EDT
Learn the remarkable shifts and evolution of best practices from the nation’s most comprehensive physician and advanced practice provider recruitment benchmark report. In this webinar, you’ll review the insightful data and process trends of nearly 170 member organizations who contributed their perspectives on the COVID-19 pandemic’s impact on hiring. Additionally, you’ll gain a competitive edge by meaningfully translating the report’s findings into value-driven discussion points for leaders and others within your organization.
Register Here and Purchase the Report
How ‘Bout This?
Staffing Word of the Week: Locum Tenens
(Edited from SIA Daily News, 10/26/2021)
Locum tenens revenue is forecast to rise 12% this year after falling 15% in 2020, according to SIA’s US Staffing Industry Forecast: September 2021 Update.
On the rebound, “locum tenens” is also this week’s Staffing Word of the Week.
SIA’s Lexicon defines locum tenens as, “Staffing of physicians, advanced practitioners (physician assistants, nurse practitioners or nurse anesthetists) or dentists on temporary assignments, which typically involves temporary relocation and staffing firm coverage of housing expenses. Locum tenens physicians are typically paid as independent contractors rather than employees.”
The Lexicon is available free online and includes terms from across the workforce solutions ecosystem.
Staffing-Related Snippets
“CVS Health Corp. says it needs doctors on its payroll to fulfill long-held ambitions of becoming a major provider of healthcare services,” The Wall Street Journal (11/3/2021) reports.
“The nation’s largest drugstore chain has worked for years to build an integrated healthcare system centered on pharmacists, in-store clinics and a massive insurance business. But until recently, the company’s plans have stopped short of including physicians.”
⭐⭐⭐
From MedPage Today’s “COVID-19 Update,” 10/5/2021: Louisiana’s largest healthcare system, Ochsner Health, will charge its employees $200 per month extra to insure unvaccinated partners or spouses covered by the hospital group’s insurance policies, citing the high cost of caring for and treating patients with COVID-19. (CBS News)
⭐⭐⭐
According to Becker’s Hospital Review, 11/3/2021, some 1,400 employees of New Hyde Park, NY-based Northwell Health either resigned or were terminated for refusing to get vaccinated against COVID-19. The departures represent less than 2% of Northwell’s workforce.